Contents
What Are ADLs and IADLs in a Home Care Setting?
Understanding Daily Living Activities in Home Care
Key Takeaways
- Activities of Daily Living (ADLs) include basic self-care tasks like bathing, dressing, and eating.
- Instrumental Activities of Daily Living (IADLs) are more complex daily tasks such as managing finances, preparing meals, and transportation.
- Challenges with ADLs or IADLs can signal a need for additional support to maintain safety, health, and independence.
- Tools like the Katz Index and Lawton-Brody IADL Scale help assess a person’s abilities and guide care planning.
- CARE Homecare offers personalized assistance with both ADLs and IADLs, helping seniors in Los Angeles and Orange County remain at home with confidence.
- Early recognition of difficulties like falls, missed medications, or isolation allows families to arrange help before problems worsen.
- CARE Homecare caregivers are trained to support daily routines with empathy, respecting each client’s dignity and preferences.
Everyday self-care tasks form the foundation of living independently. For many older adults, these basic daily activities gradually become challenging due to changes in health, mobility, or memory. Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs) are the terms professionals use to describe these essential functions.
Understanding what ADLs and IADLs include is the first step toward deciding if extra help at home would make life safer and more comfortable. This guide will clarify what these activities are, why they matter, and how in-home care services from CARE Homecare can support older adults in maintaining their dignity and independence.
What Are Activities of Daily Living (ADLs)?
Activities of Daily Living are the basic daily activities people need to manage in order to maintain their health, well-being, and physical independence. They are often the first abilities assessed when determining whether someone can safely live alone.
Here are the six main ADLs:
- Bathing and Personal Hygiene which includes washing the body, brushing teeth, and grooming hair to maintain cleanliness and prevent infection.
- Dressing – Selecting appropriate clothing for the weather or occasion and managing fasteners such as buttons and zippers.
- Eating including using utensils and feeding oneself without assistance.
- Mobility and Transferring, by being able to move safely from one position to another, such as rising from a chair or getting in and out of bed.
- Toileting including getting to and from the toilet, using it appropriately, and cleaning afterward.
- Continence – Maintaining control or managing bladder and bowel function, including handling incontinence when necessary.
These functions are so fundamental that difficulty in any area often signals a need for assistance. Many professionals use tools like the Katz Index of Independence to measure how independently a person can perform each ADL.
What Are Instrumental Activities of Daily Living (IADLs)?
Instrumental Activities of Daily Living are the more complex home management tasks that allow someone to maintain daily function and live independently. While they are not essential for basic survival, they are vital for quality of life.
Here are some common IADLs:
– Meal Preparation – Planning, cooking, and serving meals safely.
– Housekeeping – Cleaning, doing laundry, and maintaining the home environment.
– Managing Finances – Paying bills, budgeting, and keeping track of expenses.
– Transportation – Driving, using public transportation, or arranging rides to appointments.
– Medication Management – Taking the correct medications at the right times and refilling prescriptions as needed.
– Communication – While not included in the original Lawton-Brody IADL scale, modern assessments often consider the ability to use phones, email, or messaging tools essential for staying connected.
– Shopping – Acquiring groceries and household supplies regularly.
The Lawton-Brody IADL Scale is often used by clinicians to evaluate how well an individual manages these more advanced responsibilities.
Examples of ADLs and IADLs
| Category | Activity | Description |
|---|---|---|
| ADLs | Bathing and Personal Hygiene | Washing the body, brushing teeth, and grooming hair. |
| ADLs | Dressing | Selecting and putting on clothes, managing buttons, zippers, and fasteners. |
| ADLs | Eating | Using utensils to feed oneself. |
| ADLs | Mobility and Transferring | Moving safely from bed to chair, standing, or repositioning. |
| ADLs | Toileting | Getting to and from the toilet, cleaning after use. |
| ADLs | Continence | Controlling bladder and bowel functions. |
| IADLs | Meal Preparation | Planning, cooking, and serving meals safely. |
| IADLs | Housekeeping | Cleaning, laundry, organizing, and maintaining a safe home environment. |
| IADLs | Managing Finances | Paying bills, budgeting, and monitoring expenses. |
| IADLs | Medication Management | Taking medications correctly and refilling prescriptions. |
| IADLs | Transportation | Driving or arranging rides to appointments and errands. |
| IADLs | Communication | Using the phone, email, or other tools to stay in touch. |
| IADLs | Shopping | Purchasing groceries and household supplies. |
Why Do ADLs and IADLs Matter in Home Care?
The ability or inability to carry out ADLs and IADLs plays a significant role in determining how much support someone needs to live safely. These self-care tasks and independent living skills form the foundation of living independently. When a person starts to struggle with even a few, it can lead to safety risks, nutritional challenges, medication errors, and social isolation.
Assessing ADLs and IADLs helps families and professionals develop the right care plan. It becomes easier to pinpoint which services, equipment, or non-medical caregiving will be most beneficial.
At CARE Homecare, assessments are part of every personalized care plan. This approach ensures that help is tailored to each client’s abilities and preferences rather than using a one-size-fits-all approach. For clarity on what Medicare covers, visit Medicare’s guide to home health services.
Functional Evaluation and Aging Care Assessments for ADLs and IADLs
| Assessment Tool | Purpose | Helpful Resource |
|---|---|---|
| Katz Index of Independence | Measures ability to perform basic ADLs | Katz Index Overview (PDF) |
| Lawton-Brody IADL Scale | Evaluates ability to perform complex independent living tasks | Lawton IADL Scale (PDF) |
| Barthel Index | Assesses mobility and self-care tasks | Barthel Index Information (PDF) |
How CARE Homecare Supports ADLs and IADLs
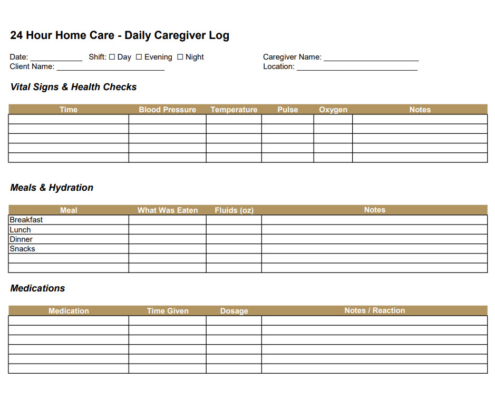
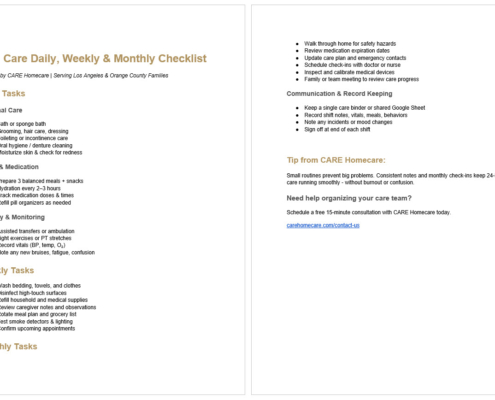
CARE Homecare offers flexible in-home assistance to support clients across a full range of basic daily activities and independent living skills. Personal care aides help with bathing, dressing, toileting, and other ADLs to keep clients comfortable and well cared for. Homemakers and companions step in to support IADLs like meal preparation, housekeeping, and transportation to medical appointments.
Care plans are designed to match each person’s unique needs and updated as those needs change over time. Families receive regular updates, and care coordinators are always available to answer questions or adjust schedules.
In Los Angeles and Orange County, CARE Homecare clients have the reassurance of knowing experienced caregivers are ready to step in, whether the need is temporary recovery support or long-term assistance with everyday tasks.
CARE Homecare Services Supporting ADLs and IADLs
| Service Type | Activities Supported |
|---|---|
| Personal Care Assistance | Bathing, dressing, toileting, mobility, eating |
| Homemaking | Housekeeping, meal preparation, shopping |
| Medication Support | Reminders, assistance with administration |
| Companionship | Social engagement, communication support |
| Transportation Assistance | Rides to medical appointments, errands, social activities |
| Family Coordination | Regular updates, care plan adjustments, support navigating insurance or benefits |
When to Consider Help with ADLs and IADLs
Deciding when to bring in help can feel overwhelming, but here are some clear signs often indicate the time is right:
- Frequent falls or near-falls
- Unintentional weight loss or signs of poor nutrition
- Missed medications or incorrect doses
- Withdrawal from social activities
- Stacks of unpaid bills or unopened mail
These challenges are common as health changes over time. Proactive planning makes it possible to address issues early and maintain a higher level of independence.
Table: Common Signs That Help May Be Needed
| Sign | Potential Risk | Possible Support |
|---|---|---|
| Frequent falls or near-falls | Injury, hospitalization | Mobility aids, caregiver supervision |
| Missed medications | Health decline, hospitalization | Medication reminders, management assistance |
| Weight loss or poor nutrition | Malnutrition, dehydration | Meal preparation support |
| Social withdrawal | Depression, isolation | Companionship services |
| Stacks of unpaid bills | Financial problems, service interruptions | Assistance managing finances, bill pay reminders |
Next Steps
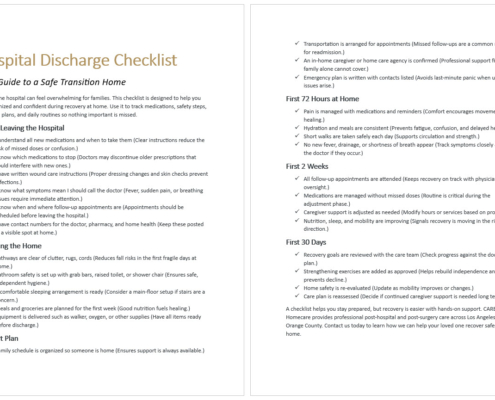
Understanding ADLs and IADLs helps families make informed decisions about the best care options for their loved ones. When these daily tasks start to feel unmanageable, in-home care can be the key to staying safe, comfortable, and engaged in life.
If you would like help evaluating which services are right for your family, the team at CARE Homecare is ready to guide you.
Contact CARE Homecare to schedule a complimentary assessment and learn how we can help.
Southern California At-Home Care & Support
If you’re exploring in-home assistance with daily living activities for yourself or a loved one in Los Angeles or Orange County, contact CARE Homecare today at (323) 851-1422 to schedule a complimentary care assessment. Our team is here to help you plan the right support to maintain safety, comfort, and independence at home.