Contents
Hospital Discharge Checklist – Free PDF Download or Print
Your Complete Guide to a Safe Transition Home
Download or Print Hospital Discharge Checklist
A safe recovery starts with preparation. Discharge day often moves quickly, and families can feel overwhelmed by instructions, paperwork and last-minute details. Our Hospital Discharge Checklist provides a clear, organized guide so nothing important is overlooked. Use it to plan questions for the care team, prepare your home and stay on track during the critical first weeks after coming home.
After downloading the checklist, you can also view our Post-Hospital Discharge Guide to Home Care Here
Why a Checklist Matters
Leaving the hospital should feel like a milestone, yet for many families it feels overwhelming. Discharge day often comes with rushed instructions, last minute decisions, and stacks of paperwork that are difficult to interpret. Hospitals discharge patients when they are medically stable, not when they are fully healed. That gap leaves families juggling medications, follow up appointments, wound care and fragile mobility without a clear plan.
A hospital discharge checklist turns uncertainty into order. By having a written guide that outlines what to ask, what to prepare and what to monitor in the first days at home, families avoid missed details that can cause setbacks. The checklist ensures every part of the transition is covered so recovery feels safe, structured and supported.
Hospital Discharge Support Across Los Angeles and Orange County by CARE Homecare
A checklist is just the first step. Having the right support at home makes all the difference. CARE Homecare provides flexible hourly and 24-hour in-home care across Los Angeles and Orange County so recovery stays safe and predictable.
Our caregivers assist with daily routines, safe mobility, meal preparation, medication reminders, companionship and home safety, giving families peace of mind from the very first night home.
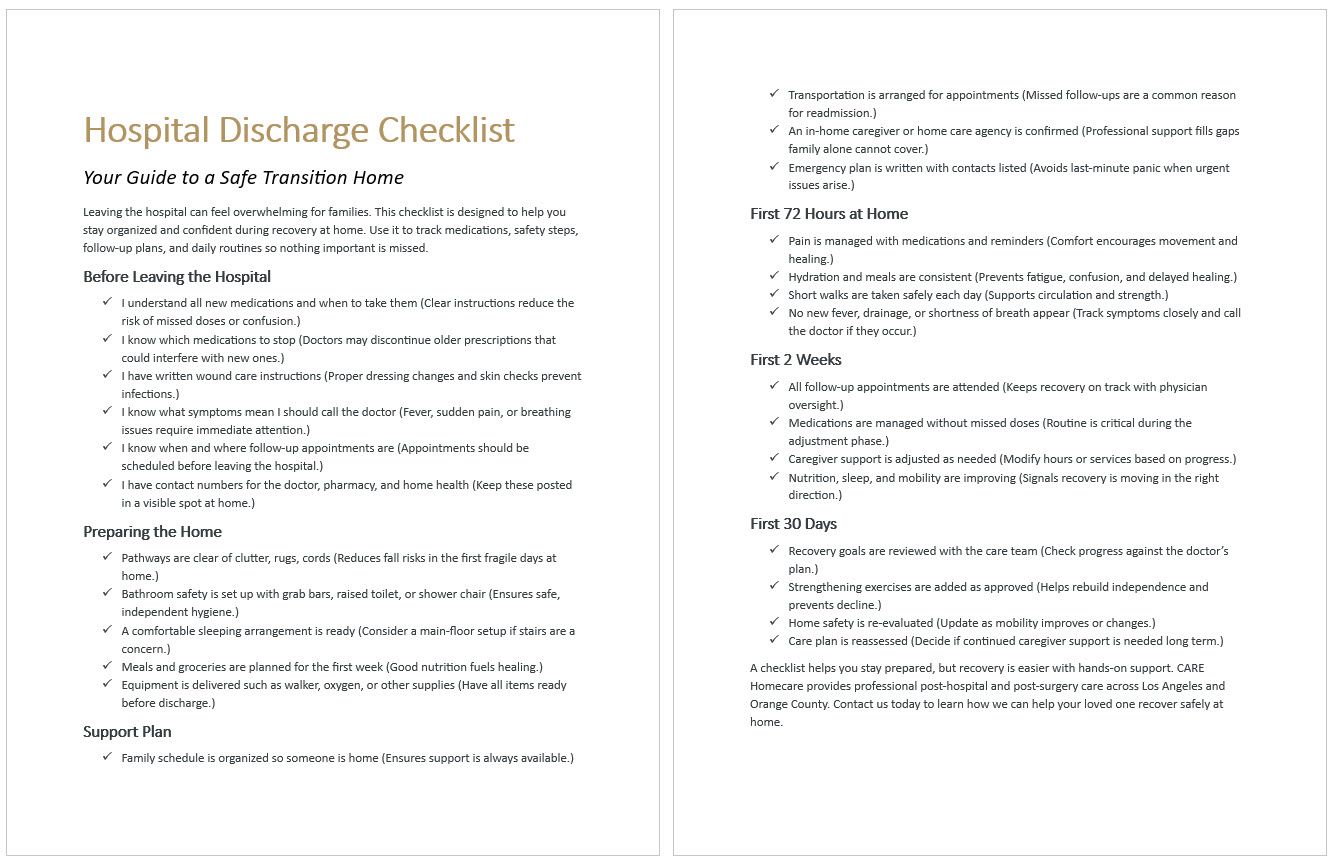
Hospital Discharge Checklist
Your Guide to a Safe Transition Home
Hospitals provide structure. There is a daily routine of meals, medication, therapy and check-ins. Patients do not have to think about what comes next. Once home, that structure collapses. Families suddenly become responsible for scheduling medications, preparing meals and monitoring for complications.
The sudden absence of professional oversight creates feelings of vulnerability.
Emotional shock is not weakness. It is a natural response to a sudden shift in responsibility and environment. By understanding why it happens, families can plan for support that makes the transition less overwhelming.
Before Leaving the Hospital
- I understand all new medications and when to take them (Clear instructions reduce the risk of missed doses or confusion.)
- I know which medications to stop (Doctors may discontinue older prescriptions that could interfere with new ones.)
- I have written wound care instructions (Proper dressing changes and skin checks prevent infections.)
- I know what symptoms mean I should call the doctor (Fever, sudden pain, or breathing issues require immediate attention.)
- I know when and where follow-up appointments are (Appointments should be scheduled before leaving the hospital.)
- I have contact numbers for the doctor, pharmacy and home health (Keep these posted in a visible spot at home.)
Preparing the Home
- Pathways are clear of clutter, rugs, cords (Reduces fall risks in the first fragile days at home.)
- Bathroom safety is set up with grab bars, raised toilet or shower chair (Ensures safe, independent hygiene.)
- A comfortable sleeping arrangement is ready (Consider a main-floor setup if stairs are a concern.)
- Meals and groceries are planned for the first week (Good nutrition fuels healing.)
- Equipment is delivered such as walker, oxygen, or other supplies (Have all items ready before discharge.)
Support Plan
- Family schedule is organized so someone is home (Ensures support is always available.)
- Transportation is arranged for appointments (Missed follow-ups are a common reason for readmission.)
- An in-home caregiver or home care agency is confirmed (Professional support fills gaps family alone cannot cover.)
- Emergency plan is written with contacts listed (Avoids last-minute panic when urgent issues arise.)
First 72 Hours at Home
- Pain is managed with medications and reminders (Comfort encourages movement and healing.)
- Hydration and meals are consistent (Prevents fatigue, confusion, and delayed healing.)
- Short walks are taken safely each day (Supports circulation and strength.)
- No new fever, drainage or shortness of breath appear (Track symptoms closely and call the doctor if they occur.)
First 2 Weeks
- All follow-up appointments are attended (Keeps recovery on track with physician oversight.)
- Medications are managed without missed doses (Routine is critical during the adjustment phase.)
- Caregiver support is adjusted as needed (Modify hours or services based on progress.)
- Nutrition, sleep and mobility are improving (Signals recovery is moving in the right direction.)
First 30 Days
- Recovery goals are reviewed with the care team (Check progress against the doctor’s plan.)
- Strengthening exercises are added as approved (Helps rebuild independence and prevents decline.)
- Home safety is re-evaluated (Update as mobility improves or changes.)
- Care plan is reassessed (Decide if continued caregiver support is needed long term.)
Understanding the Discharge Process
Families interact with several professionals during discharge. Nurses review care instructions, case managers coordinate services and discharge planners provide summaries of next steps. Each role is important, but the process often moves faster than families expect.
Typical paperwork includes a list of medications with dosages and times, follow up appointments, dietary restrictions, activity limitations, wound care directions and emergency red flag symptoms. The documents are thorough, yet not always clear to someone without a medical background.
It is also essential to understand the difference between home health care and home care. Home health is medical and requires a physician’s order. It may include skilled nursing visits, physical therapy, or wound care. Home care is non-medical and focuses on daily support such as meal preparation, medication reminders, mobility assistance and companionship. Both can work together to create a complete recovery plan.
What to Ask the Care Team Before Leaving
The hours before discharge are the best time to gather information. Families should confirm which medications are new, which to continue and which to stop. Timing and dosage should be written clearly.
If wound care or medical equipment will be required, ask for demonstrations before leaving the hospital. Whether it is changing a dressing, using a walker or managing a drain, hands-on instruction builds confidence.
Follow up appointments are another critical detail. Ask when they should take place, who will schedule them and what information should be brought.
Finally, families must know the warning signs that require immediate medical attention. Symptoms like fever, shortness of breath, chest pain, confusion or uncontrolled pain should be reported without delay.
Key Areas Families Should Prepare For at Home
Preparation at home makes recovery smoother. Safety is the first priority. Clear pathways of clutter, secure rugs and make sure lighting is adequate. Bathrooms may require grab bars, non-slip mats or a shower chair.
Nutrition and hydration are often overlooked but vital. Plan meals in advance, stock the refrigerator and keep healthy snacks available. Recovery requires consistent calories, protein and fluids.
Transportation is another factor. Families must know who will provide rides to follow up visits, therapy or lab work. Missed appointments can stall recovery or lead to readmission.
A support system should be in place. Family members may try to juggle caregiving with work, children and daily life, but professional caregivers help fill the gaps.
Emotional health also matters. Anxiety and depression are common after hospitalization. Companionship and structure help patients feel safe while regaining independence.
Why Professional Home Care Helps
Even the best checklist cannot replace hands-on support. A professional caregiver bridges the gap between medical instructions and daily living. They provide reminders for medications, prepare balanced meals, encourage safe movement, assist with ADLs like bathing or dressing and offer companionship that reduces isolation.
For families in Los Angeles, this includes navigating traffic and transportation to Cedars-Sinai, UCLA Health or Keck USC. In Orange County, caregivers support follow ups at Hoag in Newport Beach, UCI Health in Irvine or Mission Hospital in Mission Viejo. Local experience makes a difference when reliability and timing matter.
Professional home care services is not about replacing family support but strengthening it. Caregivers allow families to focus on encouragement and connection while professionals manage daily routines.
Take the Next Step
Every safe recovery begins with a plan. Our downloadable Hospital Discharge Checklist PDF gives families a simple, practical tool to stay organized from day one. It covers what to ask in the hospital, how to prepare at home and what to monitor in the first days and weeks.
If your loved one is preparing for discharge in Los Angeles or Orange County, do not face it alone. CARE Homecare provides post hospitalization care that turns instructions into action.
Contact us today to schedule care and ensure your family has the support needed for a safe, confident recovery.