Contents
The Hidden Toll of Being the “Default” Caregiver
In many families, caregiving does not arrive with a discussion or a plan. It simply lands on one person’s shoulders and quietly stays there. The default caregiver often steps in out of love, proximity, personality, or necessity. Over time, that role can turn into a full-time responsibility that reshapes identity, finances, mental health, and family dynamics. Understanding why this happens, how burnout develops, and what professional solutions actually help is essential for protecting both the caregiver and the person receiving care.
Key Takeaways
- The default caregiver role often forms without discussion, driven by proximity, gender expectations, personality traits and crisis situations rather than true availability or capacity.
- Emotional labor is as demanding as physical care, with decision-making pressure, constant vigilance and family mediation contributing heavily to caregiver stress.
- Caregiver burnout develops gradually through emotional, physical, cognitive and behavioral changes that are easy to dismiss until they begin affecting health and care quality.
- Burnout does not only harm caregivers; it directly impacts safety, emotional well-being and outcomes for the person receiving care, increasing the risk of preventable hospital readmissions.
- Families struggle to rebalance caregiving due to avoidance, minimization and entrenched family dynamics that preserve the status quo.
- Professional support such as in-home care, respite services and care coordination reduces burnout while improving consistency and safety of care.
- Sustainable caregiving requires shared responsibility, clear planning, documentation and ongoing reassessment as needs change.
- Seeking help early preserves choice, protects relationships and prevents caregiving from escalating into a health or family crisis.
Support for Default Caregivers Across Los Angeles and Orange County by CARE Homecare
Being the default caregiver should not mean carrying everything alone. CARE Homecare supports families across Los Angeles and Orange County with personalized in-home care that eases caregiver burnout while protecting the safety and dignity of your loved one. From flexible hourly support to 24-hour care, our services are designed to share the load and restore balance at home.
Our trained caregivers assist with daily routines, mobility, meal preparation, companionship, medication reminders and home safety so caregivers can step out of survival mode and families can focus on health, stability and quality of life.
Why Caregiving Duties So Often Fall on One Person
Caregiving rarely starts as an official role. It usually begins with a favor. A few rides to appointments. Helping after a hospital discharge. Managing medications for a short time. The person who steps in first is often the one who stays, especially during the high-pressure transition period described in the first 72 hours at home after hospital discharge.
Several factors consistently push one individual into the default caregiver role:
Geography plays a major role. The family member who lives closest becomes the obvious choice, even if their work schedule, health or finances make caregiving difficult. Proximity is often mistaken for availability.
Gender expectations still influence caregiving responsibilities. Daughters, wives and female relatives are more likely to be assumed caregivers, regardless of their own obligations. Cultural norms and family history quietly reinforce this imbalance.
Personality traits also matter. Organized, empathetic and reliable people are more likely to step up early. Once they demonstrate competence, families often lean on them more, unintentionally reducing their own involvement.
Crisis moments accelerate role assignment. After a hospitalization or sudden diagnosis, decisions must be made quickly. The person who handles discharge instructions or brings someone home frequently becomes the long-term coordinator of care. Resources like a family guide to home care after hospital discharge and discharge instructions explained help families understand how quickly these responsibilities can expand.
Financial dynamics can also shape caregiving roles. The person with flexible work, lower income or fewer perceived career consequences may feel pressure to absorb the role, even when the long-term cost is high. When families start comparing support options, it helps to understand what home care is and the broader home care benefits.
Over time, what began as temporary support becomes an unspoken expectation.
The Emotional and Psychological Weight of Being the Default Caregiver
Default caregivers carry more than physical tasks. They absorb emotional responsibility for decisions, outcomes and family harmony. They become the point person for doctors, agencies, siblings and emergencies.
This emotional load includes constant vigilance, fear of making mistakes, guilt about resentment and pressure to appear capable. Many caregivers report feeling trapped between their own needs and the needs of the person they care for. Over time, this tension erodes emotional resilience.
Caregivers often suppress their feelings to avoid conflict or judgment. They may hesitate to ask for help, fearing they will seem ungrateful or incapable. This isolation is one of the strongest predictors of burnout.
The emotional journey of caregiving is rarely linear. Articles like navigating the emotional journey of caregiving highlight how grief, anger, love and exhaustion can coexist, often within the same day. If your family is also coping with the shock of returning home after a major health event, the emotional shock of coming home from the hospital can help normalize what you are feeling.
Early Signs of Caregiver Burnout Families Often Miss
Burnout does not appear overnight. It builds quietly, especially when caregiving is normalized as “just what you do.”
Early emotional signs include irritability, numbness, anxiety and a loss of patience with the person receiving care. Caregivers may feel detached or resentful, then guilty for feeling that way.
Physical symptoms are often dismissed or overlooked. Chronic fatigue, headaches, sleep disruption, digestive issues and frequent illness are common. Stress hormones remain elevated for long periods, weakening immune function.
Cognitive burnout shows up as forgetfulness, difficulty concentrating and decision fatigue. Caregivers managing medications, appointments and ADLs may begin making small mistakes, which increases fear and self-blame. If you are juggling daily care tasks, it can help to revisit what counts as ADLs and IADLs so you can clearly define what must be done daily versus what can be delegated.
Behavioral changes include withdrawing from friends, neglecting hobbies, skipping medical appointments or relying on unhealthy coping mechanisms. Many caregivers stop recognizing themselves outside the caregiving role.
Unchecked burnout increases the risk of depression, anxiety disorders and serious health conditions. It also affects care quality, increasing the likelihood of hospital readmissions and crises that could have been prevented with proper support, including planning guidance like preventing readmission after surgery.
How Caregiver Burnout Impacts the Person Receiving Care
Burnout does not only harm caregivers. It directly impacts the safety, dignity and emotional well-being of the person receiving care.
Exhausted caregivers are more likely to miss medication changes, misunderstand discharge instructions or struggle with complex care needs. This is especially critical in cases involving dementia care, post-surgical recovery or chronic illness management. Resources like dementia care: a comprehensive guide for caregivers and why dementia patients thrive with in-home memory care highlight how demanding specialized care can be.
Emotional strain can alter the caregiver-patient relationship. Communication becomes strained. Patience thins. Small frustrations escalate. Both parties may feel misunderstood or resentful.
From a clinical perspective, caregiver burnout is a known contributor to preventable hospital readmissions. Families managing transitions home without adequate support often underestimate the intensity of ongoing care needs, as outlined in why discharge planning starts before you leave the hospital and the first two weeks at home after hospital discharge.
Supporting caregivers is not optional. It is essential to sustainable care.
Professional Solutions That Actually Reduce Caregiver Burnout
Professional solutions are not about replacing family involvement. They are about preserving it in a healthier, more sustainable way.
In-home care services provide hands-on assistance with ADLs, IADLs, medication reminders, mobility and companionship. Understanding what home care providers do helps families match services to real needs rather than waiting for a crisis. It can also help to understand the distinction between home care vs home health care and the differences between caregivers, home health aides, home care and home health care.
Respite care gives caregivers planned time off to rest, work or attend to their own health. Regular breaks are proven to reduce burnout and improve long-term caregiving capacity. Many families begin by exploring understanding home care services to see what support can realistically look like at home.
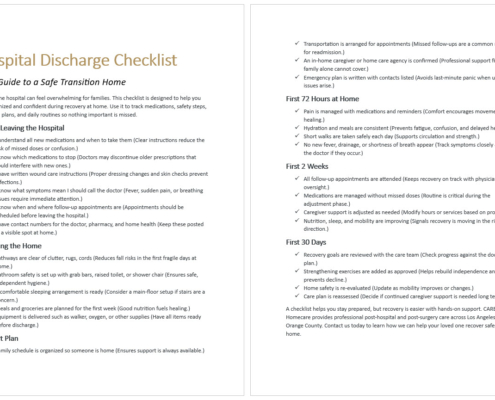
Care coordination services help manage appointments, discharge plans and communication between providers. This reduces decision fatigue and prevents errors during transitions of care. If you are currently coordinating a return home, a practical tool like the hospital discharge checklist (free PDF download) can reduce missed details.
Education is also a professional solution. Families who understand the differences between home care and home health care make better decisions and avoid unrealistic expectations.
In complex cases, especially involving cognitive decline, professional dementia care services provide structure, safety and emotional relief that family caregivers alone cannot sustain.
For families unsure where to start, learning how to choose a home care agency provides clarity and confidence. If hiring is the biggest hurdle, navigating the top challenges in hiring a senior caregiver can help you avoid common pitfalls.
Caregiving should not depend on endurance or sacrifice alone. Sustainable care requires honest conversations, realistic planning and outside support.
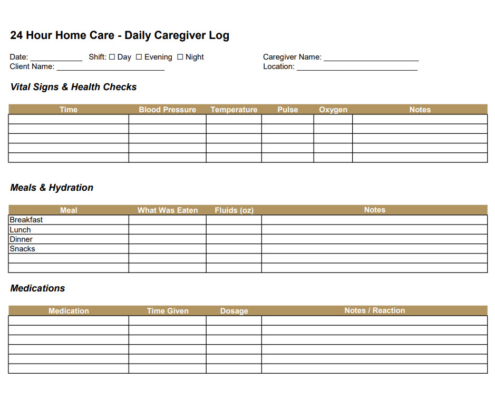
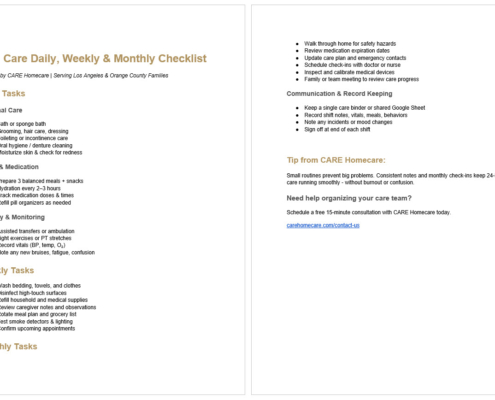
Families benefit from documenting responsibilities, scheduling regular check-ins and revisiting care plans as needs evolve. Using tools like care logs and checklists can reduce confusion and resentment, especially for intensive schedules like ‘24/7 home care documentation logs, checklists and family updates’ and the printable 24/7 care checklist PDF.
Most importantly, caregivers need permission to stop doing everything themselves. Asking for help is not failure. It is prevention.
Professional care is not a last resort. It is a protective measure that preserves health, dignity and family relationships, especially when families are weighing options like 24 hour care vs live-in care or comparing benefits of home care vs assisted living.
When to Seek Help Before Burnout Becomes a Crisis
If caregiving feels overwhelming, isolating or unsustainable, that is the moment to seek help, not later. Warning signs include declining health, emotional numbness, frequent conflict or fear about the future.
Families who act early maintain more control and choice. Those who wait often face rushed decisions during emergencies, especially after major transitions like post-hospital recovery. If your family is still in the transition window, why discharge planning starts before you leave the hospital and the first two weeks at home after hospital discharge can help you plan with fewer surprises.
Caregiving is an act of love, but love alone is not a care plan.
Contact CARE Homecare for Support That Eases the Caregiving Burden
If you are the default caregiver and feeling stretched thin, you do not have to manage everything on your own. CARE Homecare supports families across Los Angeles and Orange County with in-home care services designed to reduce burnout, share responsibility, and keep loved ones safe at home.
Whether you need short-term help after a hospital stay or ongoing support with daily care, our team will help you build a realistic plan that protects both your health and your loved one’s well-being.
Contact us through our Contact Us page to discuss a care plan tailored to your family’s needs.
You can also send us an email or give us a call.
Address: 1156 North Gardner Street, West Hollywood, CA 90046
Telephone: (323) 851-1422
Email: info@carehomecare.com